Can Painful Arthritic Shouilders Become Strong Again
Definition/Description [edit | edit source]
The shoulder complex, composed of the clavicle, scapula, and has sacrificed stability for mobility,which makes information technology vulnerable and susceptible to injury, dysfunction and instability. The most common indication for an arthroplasty is hurting that has not responded well to conservative management or a severe fracture. Depending upon the mechanism of dysfunction or injury a shoulder arthroplasty can either be a partial or full replacement.[1] [2]
Epidemiology /Etiology [edit | edit source]
The first record of shoulder arthroplasty was performed in 1894 past the French surgeon, Jean Pean.[2] The original implant consisted of a platinum and condom implant for the glenohumeral joint. Charles Neer is credited with the advancement of modern full shoulder arthroplasty (TSA), developing more modern prostheses for surgical procedures outset in the 1950's.[ii] [iii] [1]
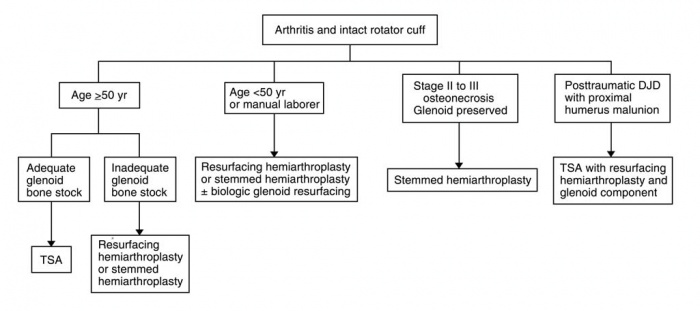
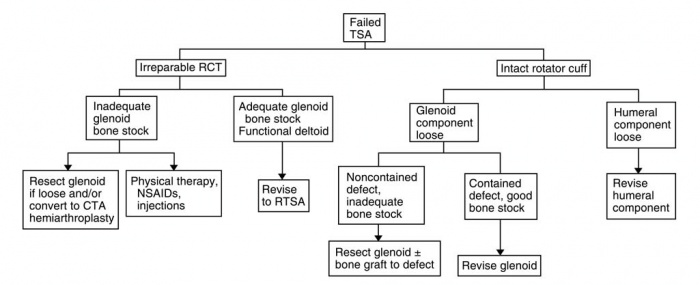
There are approximately 23,000 shoulder replacement surgeries performed each year compared to 400,000 knee replacements, and 343,000 hip replacements.[iv] This is largely due to the relative complexity of the anatomy and biomechanics of the shoulder joint. Because of the complexity of the region, in that location are multiple variations in prostheses and surgical procedures that are performed depending on the tissues that are implicated. Since Neer's initial design in 1951, more than 70 different shoulder systems have been designed for shoulder reconstruction arthroplasty.[5] The earliest shoulder replacement procedures were limited to treating proximal humeral fractures, but current implications for shoulder arthroplasty include: primary osteoarthritis, posttraumatic arthritis, inflammatory arthritis, osteonecrosis of the humeral caput and neck, pseudoparesis acquired by rotator gage deficiency, and previous failed shoulder arthroplasty. Understanding the different prosthetic options and indications for each damage is important for all practitioners in the wellness care continuum. Algorithms have been developed to clinch each patient is matched with the correct procedure and fitted with the right prosthetic option. Beneath are examples from Wiater and Fabing detailing the method for selecting the proper procedure.
Medical Direction [edit | edit source]
There are 3 main categories of shoulder reconstruction surgery: Hemiarthroplasty, total shoulder arthroplasty (TSA), and contrary full shoulder arthroplasty (rTSA).
Hemiarthroplasty [edit | edit source]

Hemiarthroplasty involves the humeral articular surface being replaced with a stemmed humeral component coupled with a prosthetic humeral head component.[iii] [5] Hemiarthroplasty is indicated when either the humerus alone is implicated, or the glenoid is not fit to back up a prosthetic. Indications include: arthritic conditions involving both the humeral head and osteonecrosis without glenoid interest, however the most common indication for this procedure are severe fractures of the proximal humerus. An optional technique is a resurfacing hemiarthroplasty that does non require a stemmed component inserted into the long shaft of the humerus, rather the humeral caput is simply resurfaced with a prosthetic component. This procedure has proven effective at managing arthritic conditions of the shoulder and is favorable for immature, able-bodied patients with worries of loosening prosthetic components.
Full Shoulder Arthroplasty [edit | edit source]
Total shoulder arthroplasty, or TSA, is a process used to supervene upon the diseased or damaged ball and socket joint of the shoulder with a prosthesis fabricated of polyethylene and metal components. In TSA, the current components of the glenoid are either a pegged or keeled high-molecular weight polyethylene cemented component.[2] These get fixated by allowing bony ingrowth through the pourous ends of the component. For some shoulders with inferior os quality, metal backing is used to increase the durability and fixation of the polyethylene component.[ii] [three] Controversy yet exists as to the stress effects metal bankroll can potentially cause on the joint.
The humeral component consists of the artificial metal humeral head attached to a metaphyseal stalk that is either fully cemented, proximally cemented, of press-fit into the humeral shaft.[2] [three] Harris et al. Found no difference in comparing micromotion between fully and proximally cemented techniques.[6]
Indications for TSA include: osteoarthritis, inflammatory arthritis, osteonecrosis involving the glenoid, and posttraumatic degenerative joint disease. The patient must also have an intact rotator gage complex, or else other prosthetic techniques would be implicated. A prospective written report by Barrett et al. found that 47 or 50 patients treated with TSA had significant decreases in pain and increases in range of motion compared to presurgical measurements.[seven] A 2004 report by Collins et al. compared conventional TSA with Hemiarthroplasty and although both groups showed significant decreases in hurting from pretreatment measurements, the TSA grouping demonstrated more increases in ROM.[viii]
In that location are several variations to the TSA procedure. Resurfacing total shoulder arthroplasty involves replacing the deteriorated bone surface of the humeral head and does not require a stemmed component inserted into the long axis of the humerus. Considering there is no stemmed humeral component, this technique is becoming a popular option. Levy and Copeland compared cementless resurfacing TSA's with standard stemmed prostheses and found comparable results.[9] An alternative for the active individual is the TSA with Biologic Glenoid Resurfacing. This procedure involves a TSA humeral component coupled with glenoid resurfacing using a grade of biologic tissue (fascia lata, anterior shoulder sheathing, Achilles tendon, menisci) and studies have shown comparable results to conventional TSA.
Comparison of published studies show some disagreement whether TSA is a superior handling to hemiarthroplasty for patients with primary osteoarthritis. A meta-assay by Radnay et al. found significantly greater hurting relief, forward meridian, gain in frontwards summit, gain in external rotation, and patient satisfaction with TSA compared with hemiarthroplasty in a total of 1,952 patients.[ten]
Opposite Total Shoulder Arthroplasty (rTSA) [edit | edit source]
A contrary total shoulder arthroplasty, or rTSA, refers to a similar procedure in which the prosthetic brawl and socket that make up the joint are reversed to treat sure complex shoulder problems.[eleven] [12] [3] rTSA involves a stemmed-humeral component containing a polyethylene humerosocket replacing the humeral caput, and a highly polished metal ball known as a glenosphere replacing the socket, or glenoid.[2] [13] One can think of this every bit the "ball and socket" components existence switched. This allows for amend fixation of the prosthetic parts and increased stability of the joint. An rTSA currently is indicated for patients suffering from osteoarthritis or compound fractures of the humerus, in conjunction with a deficiency of the rotator gage complex.[12] [14] Matsen et al. also states that an rTSA should exist considered for patients whose shoulder problems cannot exist managed using a conventional TSA.[xi] Several features make the rTSA more compatible for certain patient populations. The deep concavity of the humeral articular component, too equally the simplicity of the glenoid component, allow for better fixation of the prosthesis and fewer issues with component loosening. Bounty for rotator cuff dysfunction is made with the rTSA that typically is left unmanaged in conventional TSA. Several long term studies have been washed on the procedure with positive results.[thirteen] Early studies institute both loftier complication and revision rates, 50% and threescore% respectively, however a 2007 retrospective report by Wall et al. establish a complication charge per unit of only xix%.[11] The authors of this study also propose that rTSA tin can be used for a larger population of patients receiving a shoulder replacement, non just those with rotator cuff arthropathy. Early evidence suggests that RTSA is a viable choice for certain patient populations with more research needed in comparisons with TSA and Hemiarthroplasty.

Complications[15] [edit | edit source]
- Component Loosening - Symptomatic loosening of the glenoid and humeral component correspond one 3rd of the complications from TSA.
- Glenoid Loosening - Almost loosening is believed to be a result of aseptic loosening of the cement while new innovations of implants such every bit press-fit, plasma sprayed, and tissue-ingrowth implants are promising alternatives that could prove to be more stable than traditional cemented implants.
- Humeral Loosening - Although glenoid loosening accounts for the bulk of loosening complications, radiolucent lines of two mm or more have been seen in the humeral component and most cases are in non-cemented implants.
- Glenohumeral Instability - Second leading cause of complications in TSA
- Inductive Instability - Oftentimes associated with malrotation of the humeral component, dysfunction of the anterior deltoid, or disruption of the sutured subscapularis tendon. Most commonly this is the event of poor operative technique, poor tissue quality, inappropriate physical therapy, or the utilise of oversized components.
- Superior Instability - Progressive superior migration can be caused by failed repair of the rotator cuff, or a complete tear of the insertion of the rotator gage, but in a study of 29 TSA'south that had proximal humeral migration, just seven had a tear of the rotator cuff. This suggests that the cause is more probable a muscle imbalance with a strong deltoid and a weak, poorly rehabilitated rotator cuff. This finding helps to stress the importance of strengthening the rotator cuff in a post TSA patient.
- Posterior Instability - Excessive retroversion of the glenoid component or the humeral component can cause instability in the posterior management. Asymmetrical wear of the posterior glenoid is indicative of long standing OA and can atomic number 82 to excessive retroversion of the glenoid component.
- Inferior Instability - Ofttimes associated with TSA for proximal humeral fracture, junior instability can also be seen in patients who have had TSA to treat prosthetic revision, chronic fracture, previous osteosynthesis, or uncomplicated RA or OA. Restoration of humerus length and the proper tension of the deltoid will amend the instability.
- Rotator cuff tears - Third most frequent complication of TSA. Both operative and not-operative treatments accept been used, although benefits of operative treatment is unclear.
- Fractures - Periprosthetic, intraoperative, and postoperative fractures can filibuster postoperative rehabilitation.
- Infection - A rare only potentially devastating complication, nearly cases are associated with risk factors such as diabetes mellitus, RA, systemic lupus erythematosus, and previous operations on the shoulder.
- Neural injury - Neuropraxias are most common and tin be treated with non-operative treatment, often yielding skilful results.
- Prosthetic Complications - Occasionally complications of the implant such as dissociation of the polyethylene glenoid insert from the metallic bankroll or fracture of the keel insert tin can occur.
- Deltoid Dysfunction - Earlier procedures removed the deltoid from its origin. Today'south more common deltopectoral approach doesn't disrupt the attachment of the deltoid, resulting in less atrophy and denervation complications.
Mail Surgical Presentation/Precautions [edit | edit source]
Conventional Total Shoulder Arthroplasty [edit | edit source]
Patients will exist in a shoulder immobilizer during the twenty-four hour period for the showtime week and at night for the first calendar month, post-obit a deltopectoral interval approach.[16] [1] Iv weeks post-obit the surgery, patients volition be in a shoulder sling. In cases of certain approaches where the deltoid is removed from its zipper, precautions will vary depending of which office of the deltoid was cut besides as the general quality of the soft tissue.
Contrary Total Shoulder Arthroplasty [edit | edit source]
In the offset few days following rTSA flexion/elevation in the scapular plane tin be done passively upward to 900, but pure abduction is contraindicated as it places stress on the anterior structures of the shoulder.[12] Internal rotation is too non recommended for the start 6 weeks postoperatively to prevent dislocation. Much like the traditional TSA, the rTSA patient will be in an abduction sling/immobilizer for 3-iv weeks afterwards surgery.[13] In both traditional and reverse TSA, postoperative precautions and the progression of therapy volition exist dictated by the surgeon depending on the quality of os and soft tissue too as whatever considerations due to complications around the operation.
Physical Therapy Management [edit | edit source]
Overall recovery from total shoulder arthroplasty may accept up to one to 2 years. To date, there is express evidence detailing any postoperative rehabilitation programs. Those that are available usually consist of a progression from passive to active range of motion, after on incorporating progressive stretching and strengthening.[xvi]
The progression of the patient through the phases of rehab must be continually modified based on their underlying pathology and clinical presentation.[1] Many protocols will present with timeframes betwixt phases which should only exist used equally a guideline for the patient. The physical therapist should continuously piece of work aslope the referring surgeon in developing each patient'south specific rehabilitation protocol, with the focus on coming together certain impairment and functional criteria before progressing on to the adjacent stage. Patient didactics before and after the surgery is vital as patients must know to expect differing levels of postoperative function depending on many factors such every bit the blazon of surgical implant, status of the remaining rotator gage, and os stock of the glenoid and humeral caput.[12]
Numerous result measures tin can be used to appraise the patient throughout the grade of rehabilitation.[12] [16] [i] Some of the more unremarkably used measures are the Constant Score, Simple Shoulder Examination, and ranges of move. These tin can be used to assess patient status and progress them through varying phases of rehabilitation. The post-obit is an outline past Wilcox et al. detailing a 4 phase program for postoperative rehabilitation following total shoulder arthroplasty.[1]
Click on the thumbnail to look at Wilcox protocol.![]()
![]()
![]()
![]()
Reverse shoulder arthroplasty is a technique gaining wide popularity that requires a somewhat unlike postoperative rehabilitation protocol with its ain precautions. Boudreau et al. stresses 3 key concepts to keep in heed when developing a postoperative rehabilitation protocol: Joint protection, deltoid function, and establishing appropriate functional and ROM expectations.[12] With the rTSA, there is higher potential for instability, therefore the patient must avert placing the surgical arm in internal rotation and adduction with extension for at least the commencement 12 weeks. The deltoid will become the prime mover in shoulder elevation and its forcefulness and recruitment is disquisitional for eventual functioning of the involved extremity. Lastly, functional return and ROM will vary case by case depending on numerous pre/mail service surgical variables and the expectation of the level of functional return must be discussed with each patient. Boudreau et al. offers an extensive protocol along with their article that tin can exist accessed through the Journal of Orthopaedic and Sports Concrete Therapy.
Expected Outcomes [edit | edit source]
Many factors accept an impact on the outcomes of the postsurgical patient; they include preoperative health condition, preoperative shoulder office, historic period, gender, and social environment.[1] [16] Longevity of the prosthesis, strength, ROM, patient-reported surveys and patient reports of hurting compared to preoperative measures are commonly used every bit result measures when studies are performed. Some studies use the Unproblematic Shoulder Test (SST) to track patient progress. Since at that place is no universally accepted functional outcome measure for TSA information technology makes it hard to compare outcomes across studies. The etiological cause for TSA appears to exist the greatest indicator for prognosticating success rates postoperatively.
- Osteoarthritis: TSA is the almost successful option for pain relief and restoration of function in patients with OA who have failed conservative treatment.[1] Information technology also has the largest success rates with most serial reporting ninety%-95% of patients to be eventually pain-costless mail surgery. Most of these patients should wait to achieve acceptable functional ROM, divers every bit 140° of forward flexion.
- Rheumatoid Arthritis: Although patients with RA might have more than complicated surgical procedures, patients with advanced RA can do good greatly from TSA.[1] A study past Stewart and Kelly concluded that TSA provided reliable long term pain relief with ROM and functional improvements, although outcomes were mainly focused on surgical results such as component loosening.[17] A comparable increase in ROM is non to be expected with RA patients compared to OA and rehab should focus on performing functional activities beneath 90°, every bit they may not achieve full overhead movement.
- Rotator Cuff Arthropathy: ROM and functional outcomes of patients with cuff tear arthropathy post-obit TSA are as well typically less than patients undergoing TSA for Osteoarthritis. Virtually of these patients do not achieve forward flexion greater than ninety°.[one] Generally pain relief is even so achieved simply with a loftier rate of component loosening. It has been recommended by several studies that these patients would exist better suited for a reverse total shoulder arthroplasty with loss of rotator cuff function. [3] [12] [thirteen]
- Proximal Humeral Fractures: Due to the variability in humeral fractures, it is difficult to found baseline functional result measures for this subset of patients. Various studies have found forward flexion to exist between 92° and 102° postoperatively, with a significant decrease in hurting.[i] It is important to besides consider the underlying fracture type, as this may dictate the following course of rehab.
Key Research [edit | edit source]
Cochrane Review: Surgery for shoulder osteoarthritis (2010)
Cochrane Review: Surgical interventions for the rheumatoid shoulder (2010)
Resource [edit | edit source]
American Academy of Orthopaedic Surgeons
Medline Plus- Shoulder Replacement
Clinical Bottom Line [edit | edit source]
Total shoulder arthroplasty has get a viable selection for patients with advanced shoulder dysfunction due to a variety of different etiologies. This procedure, forth with the newer reverse full shoulder arthroplasty, tin can assist salve pain and increase function in patients when indicated. Postsurgical rehabiliation for these patients is key to obtaining successful outcomes. There is currently limited evidence and guidelines regarding postsurgical rehabilitation, therefore each patient should be evaluated on a case by case basis in strong collaboration with the patient's other healthcare providers.
References [edit | edit source]
- ↑ 1.00 1.01 i.02 1.03 i.04 1.05 1.06 i.07 1.08 1.09 1.10 Wilcox R, Arslanian Fifty, Millett P. Rehabilitation post-obit total shoulder arthroplasty. The Journal Of Orthopaedic And Sports Physical Therapy [serial online]. December 2005;35(12):821-836.
- ↑ 2.0 2.1 ii.2 2.3 2.four 2.5 ii.six Gregory T, Hansen U, Emery R, Augereau B, Amis A. Developments in shoulder arthroplasty. Proceedings Of The Institution Of Mechanical Engineers. Part H, Journal Of Engineering In Medicine [serial online]. January 2007;221(1):87-96.
- ↑ 3.0 3.1 3.2 3.three 3.4 3.v Keller J, Bak S, Bigliani L, Levine Westward. Glenoid replacement in total shoulder arthroplasty. Orthopedics [serial online]. March 2006;29(iii):221-226.
- ↑ Shoulder Joint Replacement. American Academy of Orthopaedic Surgeons Web site. http://orthoinfo.aaos.org/topic.cfm?topic=A00094. Accessed November eleven, 2010.
- ↑ v.0 5.1 Wiater J, Fabing 1000. Shoulder arthroplasty: prosthetic options and indications. The Journal Of The American Academy Of Orthopaedic Surgeons [serial online]. July 2009;17(7):415-425.
- ↑ Harris, T.E., Jobe, C.K., Dai Q.Thou. Fixation of proximal humeral protheses and rotational micromotion. Journal of Shoulder and Elbow Surgery, 2000, 9(3), 205-210.
- ↑ Barrett W, Franklin J, Jackins S, Wyss C, Matsen F. Total shoulder arthroplasty. The Periodical Of Bone And Joint Surgery. American Volume [serial online]. July 1987;69(6):865-872.
- ↑ Collins D, Harryman D, Wirth M. Shoulder arthroplasty for the treatment of inflammatory arthritis. The Journal Of Bone And Articulation Surgery. American Volume [series online]. November 2004;86-A(11):2489-2496.
- ↑ Levy O, Copeland SA: Cementless surface replacement arthroplasty (Copeland CSRA) for osteoarthritis of the shoulder. J Shoulder Elbow Surg 2004;13:266-271.
- ↑ Radnay CS, Setter KJ, Chambers Fifty, Levine WN, Bigliani LU, Ahmad CS: Total shoulder replacement compared with humeral head replacement for the handling of primary glenohumeral osteoarthritis: A systematic review. J Shoulder Elbow Surg 2007;16:396-402.
- ↑ eleven.0 eleven.1 eleven.ii Matsen 3 F, Boileau P, Walch G, Gerber C, Bicknell R. The reverse full shoulder arthroplasty. Instructional Course Lectures [serial online]. 2008;57:167-174.
- ↑ 12.0 12.i 12.2 12.iii 12.4 12.5 12.half dozen Boudreau S, Boudreau E, Higgins L, Wilcox R. Rehabilitation following reverse full shoulder arthroplasty. The Journal Of Orthopaedic And Sports Concrete Therapy [series online]. December 2007;37(12):734-743.
- ↑ 13.0 13.1 13.2 13.3 Wall B, Nové-Josserand L, O'Connor D, Edwards T, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. The Journal Of Bone And Joint Surgery. American Volume [serial online]. July 2007;89(7):1476-1485.
- ↑ Wierks C, Skolasky R, Ji J, McFarland Due east. Reverse total shoulder replacement: intraoperative and early postoperative complications. Clinical Orthopaedics And Related Inquiry [serial online]. January 2009;467(1):225-234. Available from: MEDLINE with Full Text, Ipswich, MA.
- ↑ Wirth M, Rockwood C. Complications of total shoulder-replacement arthroplasty. The Journal Of Bone And Joint Surgery. American Volume [serial online]. Apr 1996;78(iv):603-616.
- ↑ 16.0 16.one sixteen.ii sixteen.3 Boardman North, Cofield R, Bengtson K, Little R, Jones M, Rowland C. Rehabilitation after full shoulder arthroplasty. The Journal Of Arthroplasty [serial online]. June 2001;xvi(4):483-486.
- ↑ Stewart M, Kelly I. Total shoulder replacement in rheumatoid disease: vii- to 13-twelvemonth follow-up of 37 joints. The Journal Of Bone And Joint Surgery. British Book [serial online]. January 1997;79(ane):68-72.
Can Painful Arthritic Shouilders Become Strong Again
Source: https://www.physio-pedia.com/Total_Shoulder_Arthroplasty

0 Response to "Can Painful Arthritic Shouilders Become Strong Again"
Post a Comment